Smart Patient Bed: Pressure Ulcer Detection
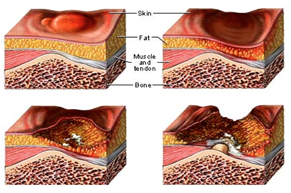 |
Pressure ulcer, also popularly known as bedsore, is one of the most common and serious problems facing patient health care in hospitals and people with disabilities. These occur on the areas of the skin and tissues that are constantly under pressure. Although people with paralysis are susceptible, anyone who is bedridden and is unable to change positions without help can develop bedsores. The blood circulation to the vulnerable parts of the body is cut off and without adequate blood flow and oxygen supply results in necrosis and tissue damage. The bedsores have been found to develop and progress rapidly due to cell breakdown and are often difficult to heal. The most important step to prevent bedsore is by avoiding prolonged pressure on any single part of the body, especially the known pressure points. The pressure sores cannot be eliminated and only be delayed when the patients are immobile. Also, the pressure points can only be redistributed to another portion of the body by using an intelligent pressure redistribution scheme. The complex commercially available pressure relieving systems including the hospital beds and the sleep number beds are expensive and often do not work well. In this research, we have developed a low cost, low power Texas Instruments (TI) MSP430 microcontroller based self contained system for pressure detection and monitoring in Patient Beds. This system paves the way for providing the information that can be used in future redistribution of pressure points.
Patient Monitoring and Connected Healthcare
Population ageing is an ever increasing trend. There are a plethora of diseases and illnesses associated with ageing. This has increased the healthcare costs tremendously. Minimizing the healthcare costs has become the economic priority for the healthcare providers. This has become the driving force to look out for innovative solutions for patient care and patient monitoring outside the hospital setting. Studies have indicated that patient care outside the hospital environment has immense potential to reduce unnecessary hospitalizations, increase the quality of life, manage the disease effectively and eventually reduce the burden on the ever-rising healthcare costs. Current advancements in sensor technology, wireless communication and miniaturized electronic devices have made unobtrusive home patient monitoring a possibility. Home patient monitoring can give an early warning to heart irregularities or chronic conditions such as high blood pressure which can lead to a heart attack or stroke. We have built an infrastructure for the patient monitoring system which provides complete end to end solution. The infrastructure contains monitoring devices that are equipped with wireless capability to relay the vital physiological data to a central health server using both PC based gatewaydevice and mobile gateway device. We have also built web application to retrieve the captured biological information for presentation and trending analysis.
Propagation and Transmission Characterization for Use of Wireless around Human Body
Recent advancements in miniaturization of electronic devices and in wireless technology have led to wearable telemedicine systems. These systems involve the interaction with the human body. The human body can be considered as a large lossy medium with electromagnetic properties. These properties vary significantly with the tissue type and the frequency. Antenna and transceivers for wearable telemedicine systems cannot be designed without understanding and investigating the electromagnetic properties of the body. Also presence of human body in the vicinity of the body-worn antennas affects the performance characteristics such as radiation pattern, feed point impedance and efficiency of the body worn antennas. Our goal is to explore the radio frequency channel propagation and characterization in the proximity of human body to mitigate the path loss and find optimum antenna placement for effective communication.
Sleep Management and Sleep Apnea
Sleep Apnea Syndrome (SAS) is a common but rarely diagnosed disorder which is characterized by repetitive episodes of cessation of breathing during sleep which leads to hypoxemia and sleep disruption. The consequences of arousals and resumption of ventilation response to hypercapnea and hypoxia result in excessive daytime sleepiness, neurocognitive dysfunction, development of cardiovascular disorders, high blood pressure and heart rate, metabolic dysfunction, chronic stress levels with systemic and pulmonary hypertension, and on the whole, leading to depression and an impaired quality of life. The Obstructive SAS (OSAS) and Central SAS (CSAS) are two types of Sleep Apnea Syndrome. While the CSAS is a breathing disorder caused by reduced respiratory drive from the central nervous system to the muscles of respiration and is common in patients with heart failure and cerebral neurologic diseases, the OSAS, on the other hand, is a prevalent disorder due to upper airway obstruction and intrathoracic pressure, especially in cases of obesity and craniofacial abnormalities, in which there is snoring, repetitive apneic episodes. The diagnosis of SAS requires assessment of subjective symptoms and apneic episodes during sleep documented by sleep monitoring as in polysomnography. A variety of physiological signatures such as ECK, EEG, EOG, EMG, pulse, respiration, thoracic and abdominal movement, and Oxygen saturation are analyzed in order to establish the presence of apnea. The current technology for detection involves a cumbersome process with the subject connected to multiple leads and wires thereby restricting and possibly disrupting the subject�s natural sleeping conditions. The objective is to be able to detect and establish the presence of sleep apnea as early as possible with minimal signals through remote home monitoring systems.
Chronic Disease Management: Obesity
Obesity and overweight is a serious epidemic that plagues today�s society. Over 30% of the adult population in the United States is obese with two thirds overweight or obese. This epidemic carries an increased risk for various co-morbidities and chronic conditions such as diabetes, hypertension, cardiovascular disease, joint and back pain, and inflammation. Further, an immense financial burden is imposed on the healthcare system to treat these co-morbidities. The problem of overweight and obesity is analogous to a bathroom sink that is overflowing. Treating the results is like using a towel to dry the floor, which might provide some temporary relief, but does not solve the problem. Treating the source, obesity, is like turning off the sink and unclogging it.(Maybe not necessary) Weight gain is a product of an imbalanced Energy Balance, where Energy Balance is the relation of Energy Intake (EI) versus Energy Expenditure (EE). EI is the amount of energy an individual acquires through ingestion of solids and liquids. EE is the amount of energy an individual expends through activity and basic bodily functioning such as organ maintenance. Weight loss can be achieved through lowering EI and/or increasing EE such that more energy is consumed than ingested; weight maintenance is achieved by keeping EI and EE roughly equal. In practice, however, the solution is not this straight forward, as there is a myriad of possible causes for the energy imbalance that vary per individual. Most weight loss and weight maintenance therapies focus on changing EI and EE. Our goal is to provide automated detection and monitoring of EI and EE to aid in an individualized therapy. EI can be detected using microphone and strain sensors to detect instances of food/liquid consumption. Detection of EE is possible using sensors such as accelerometers, pedometers, and heart rate monitors as well as formulas based on an individual�s height, weight, gender, and age. These sensors can be incorporated in an existing wireless monitoring system, which includes various other biological sensors such as a digital weight scale and blood pressure monitor. This system offers a snapshot of each individual undergoing weight loss therapy which allows assessment and adjustment to the prescribed therapy to increase effectiveness.